HEALTH– A type of cancer that originates from the cell of the cervix Located in the lower part of the uterus connecting the vagina in women, Cervical Cancer has pose a lot of treats among women and overtime position itself to be one of the deadliest. The cancer can develop from exposure to the human papillomavirus (HPV) which is a sexually transmitted infection.
Largely, the deadly disease has two types; the squamous cell carcinoma- wherein the cancer originates in the outer lining of the cervix containing the squamous cells and adenocarcinoma- which is the lesser prevalent form and originates in the column-shaped glandular cells.
It is usually caused by the genetic mutation of cells turning them from normal to abnormal cells in the cervix. Meanwhile, the exact cause of the mutation is yet unascertained by medical practitioners. Some of the factors that increases the risk of cervical cancer are: Having multiple sexual partners, sexual intercourse at an early age, sexually transmitted diseases and infections, excessive smoking and having weak or inefficient immune system.
Overtime, it has been proven that regular screening and vaccinations can help prevent the development of this cancer.
However, scientist have predicted the end of women’s health treat, cervical cancer after the success of the human papillomavirus (HPV) vaccination.
The vaccination was introduced in the year 2009 for school girls and was extended to boys for the first time this year.
According to The Lancet, a review of 65 studies covering 60million people has revealed a clear drop in number of cases of HPV and pre-cancerous cells.
“We identified 1702 potentially eligible articles for this systematic review and meta-analysis, and included 65 articles in 14 high-income countries: 23 for HPV infection, 29 for anogenital warts, and 13 for CIN2+. After 5–8 years of vaccination, the prevalence of HPV 16 and 18 decreased significantly by 83% (RR 0·17, 95% CI 0·11–0·25) among girls aged 13–19 years, and decreased significantly by 66% (RR 0·34, 95% CI 0·23–0·49) among women aged 20–24 years. The prevalence of HPV 31, 33, and 45 decreased significantly by 54% (RR 0·46, 95% CI 0·33–0·66) among girls aged 13–19 years. Anogenital wart diagnoses decreased significantly by 67% (RR 0·33, 95% CI 0·24–0·46) among girls aged 15–19 years, decreased significantly by 54% (RR 0·46, 95% CI 0.36–0.60) among women aged 20–24 years, and decreased significantly by 31% (RR 0·69, 95% CI 0·53–0·89) among women aged 25–29 years. Among boys aged 15–19 years anogenital wart diagnoses decreased significantly by 48% (RR 0·52, 95% CI 0·37–0·75) and among men aged 20–24 years they decreased significantly by 32% (RR 0·68, 95% CI 0·47–0·98). After 5–9 years of vaccination, CIN2+ decreased significantly by 51% (RR 0·49, 95% CI 0·42–0·58) among screened girls aged 15–19 years and decreased significantly by 31% (RR 0·69, 95% CI 0·57–0·84) among women aged 20–24 years”.
“This updated systematic review and meta-analysis includes data from 60 million individuals and up to 8 years of post-vaccination follow-up. Our results show compelling evidence of the substantial impact of HPV vaccination programmes on HPV infections and CIN2+ among girls and women, and on anogenital warts diagnoses among girls, women, boys, and men. Additionally, programmes with multi-cohort vaccination and high vaccination coverage had a greater direct impact and herd effects”.
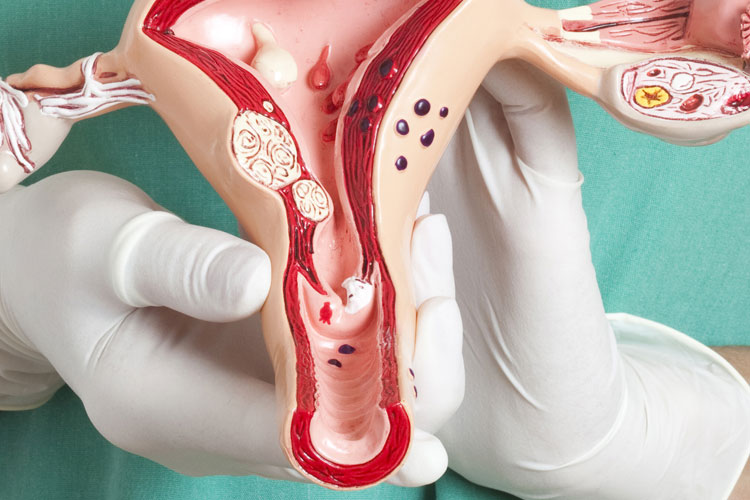
Nonetheless, many uterus will have their way of carrying babies, as surgical removal of uterus still remains the prescribed option for early stage cervical cancer treatment, according to research, this serves not just the treatment of cervical cancer but also as a preventive measures against recurrence.
The surgery may be either a simple hysterectomy – which is removal of the cancer along with the cervix, uterus and is an option only in the early stages of the disease. A radical hysterectomy may be performed with later stage cancers wherein the cervix, uterus, a part of the vagina and lymph nodes are also removed along with the cancer.